Improving Mental Healthcare: Addressing Systemic Issues

Table of Contents
Lack of Access to Affordable Mental Healthcare
The current system presents significant barriers to accessing mental healthcare, particularly for vulnerable populations. These barriers manifest in two primary forms: geographic limitations and financial constraints.
Geographic Barriers
Unequal distribution of mental health professionals creates significant access challenges, especially in rural and underserved communities. Many individuals lack access to essential services due to:
- Lack of transportation: Limited public transport and long distances to mental health facilities make regular appointments impossible for many.
- Limited availability of telehealth services: While telehealth offers a potential solution, its accessibility is uneven, often hindered by unreliable internet access and a lack of digital literacy.
- Long wait times for appointments: Even when services are available geographically, long wait times can deter individuals from seeking help, potentially exacerbating their conditions.
For instance, rural counties in many states have significantly fewer psychiatrists per capita than urban areas, leaving residents with limited options and lengthy travel times to access care. Implementing mobile mental health clinics and expanding telehealth initiatives with robust internet access support could help bridge this gap.
Financial Barriers
The high cost of mental healthcare is a major impediment for many, leaving them unable to afford necessary treatment. Key factors contributing to this problem include:
- High cost of therapy, medication, and hospitalization: Therapy sessions, prescription medications, and inpatient treatment can be prohibitively expensive.
- Inadequate insurance reimbursement rates: Many insurance plans offer limited coverage for mental health services, leaving individuals with significant out-of-pocket expenses.
- Lack of sliding-scale fees: The absence of flexible payment options further limits access for low-income individuals.
The consequences are dire, particularly for individuals from lower socioeconomic backgrounds. Addressing this requires a multi-pronged approach, including increased government funding for mental health services, stronger affordable care acts with comprehensive mental health coverage, and a wider availability of community-based mental health services offering sliding-scale fees.
Stigma and Societal Attitudes Towards Mental Illness
Negative societal attitudes and the pervasive stigma surrounding mental illness significantly hinder help-seeking behavior.
The Impact of Stigma
The fear of judgment, discrimination, and social repercussions prevents many individuals from seeking professional help. This fear manifests as:
- Fear of losing jobs, relationships, or social standing: The stigma associated with mental illness can lead to job discrimination, relationship strain, and social isolation.
- Reluctance to seek help due to shame or embarrassment: Individuals may feel ashamed or embarrassed to admit they are struggling with their mental health.
- Societal misconceptions and negative stereotypes: Harmful stereotypes perpetuate misconceptions and fuel discrimination against individuals with mental illnesses.
Overcoming this requires a concerted effort to challenge these misconceptions. Sharing personal stories, promoting positive representations of mental health in media, and providing education and resources can help reduce stigma.
Promoting Mental Health Literacy
Increasing public awareness about mental health conditions is crucial to reducing stigma and encouraging help-seeking behavior. Key strategies include:
- School-based mental health education: Integrating mental health education into school curriculums can foster understanding and reduce stigma from a young age.
- Public awareness campaigns: Well-designed campaigns can educate the public about mental health conditions, symptoms, and available treatment options.
- Training for healthcare professionals and community members: Equipping healthcare professionals and community members with the knowledge and skills to address mental health concerns is essential.
Successful campaigns like those run by the National Alliance on Mental Illness (NAMI) demonstrate the positive impact of raising awareness and promoting understanding.
Shortage of Mental Health Professionals
A severe shortage of qualified mental health professionals exacerbates the challenges in accessing care.
The Workforce Crisis
The shortage of psychiatrists, psychologists, therapists, and other mental health professionals creates long wait times and limited access to quality care. Factors contributing to this crisis include:
- High training costs: The extensive education and training required for mental health professions are costly, deterring many potential candidates.
- Limited training opportunities: A lack of available training positions further restricts the pipeline of new professionals.
- Burnout and high attrition rates among professionals: The demanding nature of the work and lack of adequate support lead to burnout and high turnover rates.
This shortage results in inadequate care for those who need it most. Longer wait times, limited appointment availability, and reduced access to specialized services are the direct consequences.
Expanding the Mental Health Workforce
Addressing the shortage requires a multifaceted approach:
- Investing in mental health training programs: Increased funding for education and training programs can attract more individuals to the field.
- Expanding telehealth options: Telehealth can improve access to care in underserved areas and reduce the burden on existing professionals.
- Creating supportive work environments for mental health professionals: Improving working conditions, providing adequate compensation, and reducing burnout are crucial to retaining experienced professionals.
Initiatives focused on loan repayment programs, mentorship opportunities, and improved working conditions are essential for attracting and retaining a robust mental health workforce.
Conclusion
Improving mental healthcare requires a comprehensive approach that tackles systemic issues head-on. The lack of access to affordable care, the pervasive stigma surrounding mental illness, and the critical shortage of mental health professionals all contribute to a healthcare system that fails to meet the needs of millions. By addressing these systemic issues, we can create a more equitable and supportive system for everyone. Let's work together to improve mental healthcare for all. Advocate for policy changes that expand access, support mental health organizations working to reduce stigma, and seek help if you or someone you know is struggling. Improving mental healthcare is a collective responsibility.

Featured Posts
-
 Lotto 6aus49 Vom 12 April 2025 Alle Ergebnisse Auf Einen Blick
May 03, 2025
Lotto 6aus49 Vom 12 April 2025 Alle Ergebnisse Auf Einen Blick
May 03, 2025 -
 Tory Chairmans Criticism Of Farage Fuels Conflict With Reform Uk
May 03, 2025
Tory Chairmans Criticism Of Farage Fuels Conflict With Reform Uk
May 03, 2025 -
 Is A Play Station Showcase Finally Coming Ps 5 Fans React
May 03, 2025
Is A Play Station Showcase Finally Coming Ps 5 Fans React
May 03, 2025 -
 Leaked Fortnite Icon Skin Details And Release Date
May 03, 2025
Leaked Fortnite Icon Skin Details And Release Date
May 03, 2025 -
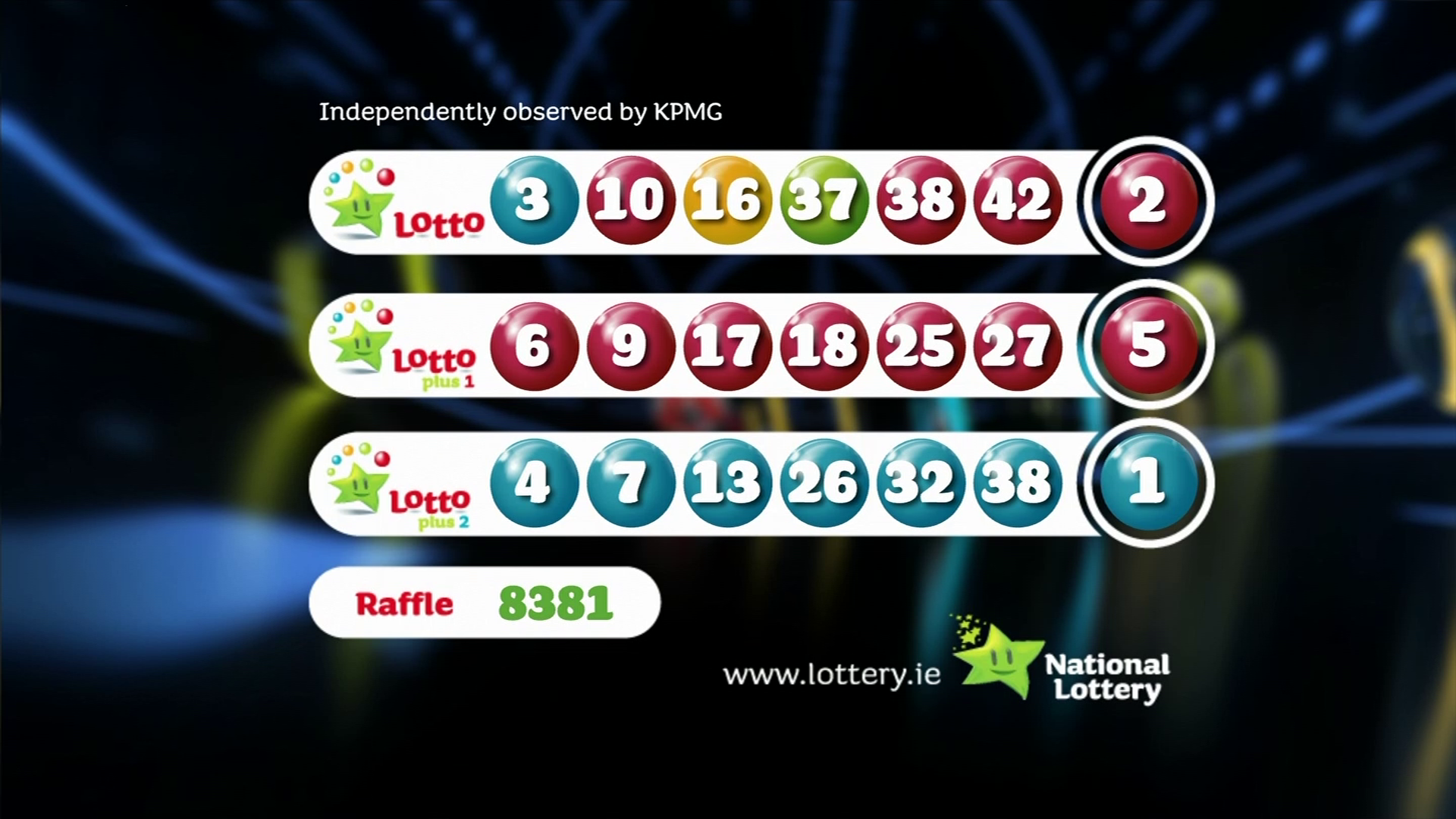 Official Lotto Results Wednesday 30 April 2025
May 03, 2025
Official Lotto Results Wednesday 30 April 2025
May 03, 2025
