Improving Access To Mental Healthcare In Ghana: Tackling The Psychiatrist Deficit

Table of Contents
The Scope of the Psychiatrist Deficit in Ghana
The psychiatrist shortage in Ghana is alarming. The current psychiatrist-to-population ratio is drastically below the recommended levels set by the World Health Organization (WHO). Precise figures vary depending on the source, but estimates consistently reveal a severe deficit. For example, [cite a reliable source, e.g., a Ghanaian Ministry of Health report or WHO data], suggests a ratio of [insert ratio] psychiatrists per 100,000 people, far below the WHO's recommended ratio of [insert WHO recommended ratio]. This disparity is further exacerbated by an uneven distribution of existing psychiatrists. Urban areas tend to have a higher concentration of mental health professionals, leaving rural communities severely underserved and facing significant barriers to accessing care. This geographical disparity creates a critical mental health gap, leaving many individuals without access to essential services.
- Current psychiatrist-to-population ratio in Ghana: [Insert data with citation]
- Regional disparities in psychiatrist distribution: [Describe urban-rural disparities with data and examples]
- Comparison with psychiatrist ratios in other African countries or global averages: [Include comparative data with citations]
- Impact of the shortage on access to essential mental health services: Limited access to diagnosis, treatment, medication, and follow-up care.
Consequences of Inadequate Access to Mental Healthcare
The consequences of inadequate access to mental healthcare in Ghana are far-reaching and devastating. Untreated mental illness leads to a significant increase in the burden of disease, impacting individuals, families, and society as a whole. The lack of access contributes to:
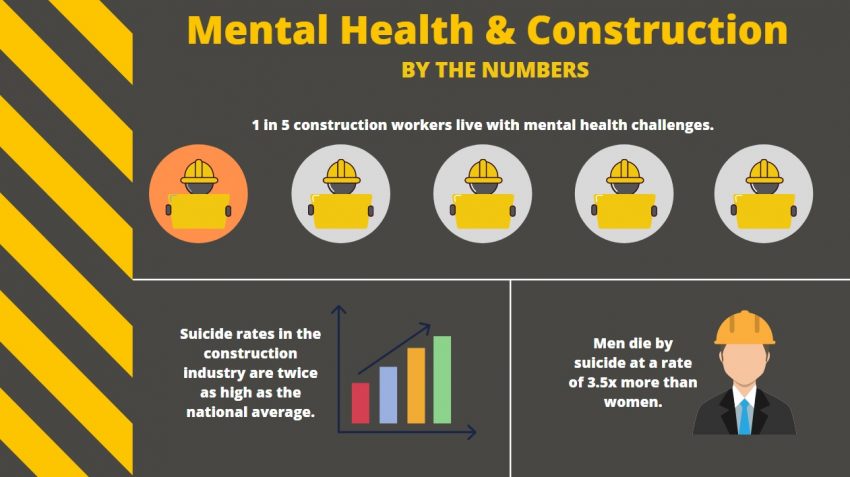
- Increased rates of suicide and self-harm: The absence of timely intervention can lead to tragic outcomes. [Insert statistics on suicide rates in Ghana with citation].
- Higher prevalence of untreated mental illness: Many individuals suffer silently, their conditions worsening without proper care. This can lead to chronic disability and reduced quality of life.
- Economic burden on families and the healthcare system: The cost of untreated mental illness includes lost productivity, increased healthcare utilization for managing complications, and the financial strain on families providing informal care.
- Social consequences of untreated mental health conditions: Stigma surrounding mental illness further compounds the problem, preventing individuals from seeking help and leading to social isolation and discrimination.
Strategies for Improving Access to Mental Healthcare in Ghana
Addressing the psychiatrist deficit and improving access to mental healthcare requires a multi-pronged approach involving several key strategies:
- Investment in medical training programs for psychiatrists: Increasing the number of trained psychiatrists through scholarships, targeted training programs, and improved residency opportunities is crucial. This should include attracting and retaining qualified professionals.
- Expanding the role of non-physician mental health professionals: Training and empowering nurses, social workers, and community health workers to provide basic mental healthcare services can significantly increase access in underserved areas.
- Implementing telehealth solutions for remote areas: Utilizing technology to deliver mental healthcare services remotely can overcome geographical barriers and improve access in rural communities.
- Community-based mental health programs: Developing and implementing community-based programs can bring mental healthcare closer to individuals, reducing stigma and improving help-seeking behavior.
- Public awareness campaigns to reduce stigma: Addressing the pervasive stigma surrounding mental illness is critical to encouraging help-seeking behavior. This requires comprehensive public awareness campaigns to educate the population about mental health conditions and available resources.
- Strengthening national mental health policies and legislation: A strong policy framework is essential to guide resource allocation, service delivery, and training initiatives. This includes allocating adequate funding for mental health services.
The Role of International Collaboration and Funding
International collaboration and funding are vital for achieving sustainable improvements in mental healthcare access in Ghana. Partnerships with international organizations like the WHO, UNICEF, and NGOs with experience in mental health can provide:
- Securing international grants and funding: Securing funding for training programs, infrastructure development, and community-based initiatives is essential.
- Partnerships with international organizations (e.g., WHO, UNICEF): These partnerships can provide technical expertise, capacity building, and financial support.
- Capacity building through international collaborations: Sharing best practices and expertise from other countries with successful mental health programs can significantly enhance Ghana's capacity.
- Sharing best practices from other countries: Learning from successful models in other countries can inform the development of effective strategies for Ghana.
Conclusion
The psychiatrist shortage in Ghana poses a critical threat to the mental well-being of its citizens. The consequences of inadequate access to mental healthcare are far-reaching and devastating, impacting individuals, families, and the nation as a whole. To address this urgent crisis, a multifaceted approach is necessary, encompassing increased investment in training, expansion of the mental health workforce, leveraging technology, strengthening community-based initiatives, addressing stigma, and securing international collaborations and funding. We must all support initiatives for improving mental healthcare access in Ghana, advocate for increased funding for mental health services in Ghana, and join the movement to tackle the psychiatrist deficit in Ghana. The future of mental health in Ghana depends on our collective commitment to action.

Featured Posts
-
 Bila Je Prva Ljubav Zdravka Colica Kad Sam Se Vratio Ti Si Se Udala
May 02, 2025
Bila Je Prva Ljubav Zdravka Colica Kad Sam Se Vratio Ti Si Se Udala
May 02, 2025 -
 Investing In Xrp Ripple A Look At The Current Market
May 02, 2025
Investing In Xrp Ripple A Look At The Current Market
May 02, 2025 -
 Winning Lotto And Lotto Plus Numbers Saturday April 12 2025
May 02, 2025
Winning Lotto And Lotto Plus Numbers Saturday April 12 2025
May 02, 2025 -
 Check The Daily Lotto For Wednesday April 16th 2025
May 02, 2025
Check The Daily Lotto For Wednesday April 16th 2025
May 02, 2025 -
 Colorado Buffaloes Visit No 9 Texas Tech After Toppins 21 Point Game
May 02, 2025
Colorado Buffaloes Visit No 9 Texas Tech After Toppins 21 Point Game
May 02, 2025
Latest Posts
-
 The Urgent Mental Health Needs Of Young People In Canada Lessons From A Global Commission
May 03, 2025
The Urgent Mental Health Needs Of Young People In Canada Lessons From A Global Commission
May 03, 2025 -
 The Impact Of Cost And Stigma On Mental Healthcare Access Low Claim Rates Explained
May 03, 2025
The Impact Of Cost And Stigma On Mental Healthcare Access Low Claim Rates Explained
May 03, 2025 -
 Low Mental Health Insurance Claims Exploring The Barriers To Care
May 03, 2025
Low Mental Health Insurance Claims Exploring The Barriers To Care
May 03, 2025 -
 Mental Health Claim Rates High Costs And Stigma Limit Access
May 03, 2025
Mental Health Claim Rates High Costs And Stigma Limit Access
May 03, 2025 -
 Mental Health Courses By Government Ignou Tiss Nimhans And More
May 03, 2025
Mental Health Courses By Government Ignou Tiss Nimhans And More
May 03, 2025
