Co-occurring ADHD, Autism, And Intellectual Disability: A Comprehensive Study
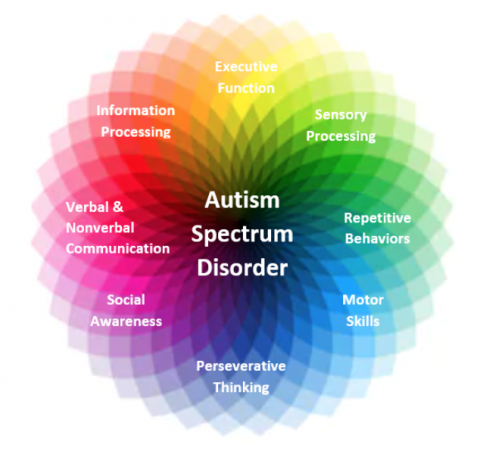
Table of Contents
Diagnostic Challenges and Comorbidity
The accurate diagnosis of co-occurring ADHD, ASD, and ID presents significant challenges due to substantial symptom overlap. These conditions often share common features, making differentiation difficult and requiring careful consideration by experienced professionals.
Overlapping Symptoms
Many symptoms are shared across ADHD, ASD, and ID, hindering precise diagnosis. This overlap necessitates comprehensive assessment.
- Inattention: Difficulty focusing, easily distracted, struggling to follow instructions. These are hallmarks of both ADHD and some presentations of ASD and ID.
- Social Communication Difficulties: Challenges with social interaction, understanding nonverbal cues, and engaging in reciprocal communication are present in both ASD and, to varying degrees, in ID.
- Intellectual Limitations: Cognitive deficits impacting learning, problem-solving, and adaptive functioning are central to ID, but can also be present in individuals with severe ASD or ADHD.
The need for comprehensive assessment tools and experienced professionals who understand the nuances of these co-occurring conditions cannot be overstated. A thorough evaluation should involve multiple assessments and observations across different settings.
Differential Diagnosis
Distinguishing between ADHD, ASD, and ID is critical for developing appropriate interventions. Each condition presents unique strengths and weaknesses, requiring personalized support.
- DSM-5 Criteria: Accurate diagnosis relies on applying the specific diagnostic criteria outlined in the DSM-5 for each condition. This involves careful review of developmental history, behavioral observations, and standardized assessments. For example, differentiating between inattention stemming from ADHD versus that resulting from cognitive limitations in ID requires a nuanced understanding of the individual’s overall profile.
- Developmental History: A detailed developmental history is essential for identifying the onset and progression of symptoms, further clarifying the diagnosis. Early intervention services may be crucial in this context.
- Standardized Assessments: Utilizing standardized assessments like the Wechsler Intelligence Scales, ADOS (Autism Diagnostic Observation Schedule), and Connors rating scales are crucial for obtaining objective data and supporting the diagnostic process.
A thorough differential diagnosis ensures that support services are targeted appropriately and maximize positive outcomes.
Prevalence of Co-occurrence
Studies indicate a high prevalence of co-occurring ADHD, ASD, and ID.
- Statistics: Research consistently demonstrates a significantly higher rate of co-occurrence compared to the expected rate based on individual prevalence. Exact figures vary depending on the population studied and diagnostic methods employed.
- Research Studies: Multiple large-scale epidemiological studies have documented the elevated comorbidity rates, highlighting the importance of acknowledging this population in clinical practice and research.
This high comorbidity rate may be due to shared genetic factors, similar underlying neurological mechanisms, or an overlap in environmental risk factors. Further research is needed to fully elucidate these contributing factors.
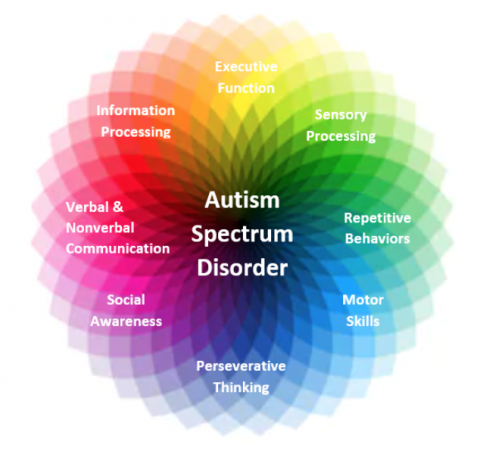
Common Characteristics and Behavioral Presentations
Individuals with co-occurring ADHD, ASD, and ID often exhibit specific patterns of behavior and challenges in adaptive functioning.
Adaptive Functioning
Significant challenges in daily living skills are common.
- Communication: Difficulties understanding and expressing themselves verbally and nonverbally.
- Self-Care: Challenges with personal hygiene, dressing, and eating independently.
- Social Interaction: Significant difficulties forming and maintaining relationships, understanding social cues, and navigating social situations.
These challenges can significantly impact their ability to participate in education, employment, and community life. Support services focusing on improving these skills are paramount.
Emotional and Behavioral Difficulties
This population experiences an increased risk of emotional and behavioral problems.
- Anxiety and Depression: High prevalence of anxiety disorders and depressive symptoms.
- Aggression: Self-directed or other-directed aggression, challenging behaviors, and self-injurious behavior.
- Tantrums and Meltdowns: Difficulty managing emotions and regulating behavior resulting in emotional outbursts.
Addressing these emotional and behavioral difficulties is essential through appropriate interventions that involve psychological support, behavior modification strategies, and, in some cases, medication management.
Sensory Sensitivities
Sensory processing difficulties are frequently observed.
- Oversensitivity: Extreme reactions to certain sounds, textures, lights, or smells.
- Undersensitivity: Reduced awareness or response to sensory input.
- Sensory Seeking: A need for repetitive sensory experiences.
These sensitivities can significantly impact daily functioning, learning, and social participation. Creating supportive and sensory-friendly environments is crucial.
Effective Interventions and Support Strategies
Effective interventions for co-occurring ADHD, ASD, and ID require a multifaceted approach.
Individualized Education Programs (IEPs)
Tailored education plans are critical.
- Accommodations: Modifications to teaching methods, classroom environment, and assessment procedures to meet the individual's specific needs.
- Modifications: Adjustments to curriculum content and expectations to ensure appropriate challenge and support.
Collaboration between educators, therapists, and parents is essential for developing and implementing effective IEPs.
Behavioral Interventions
Behavioral therapies are vital for managing challenging behaviors and improving adaptive skills.
- Applied Behavior Analysis (ABA): Focuses on breaking down complex behaviors into smaller, manageable steps and using positive reinforcement to promote desired behaviors.
- Positive Behavior Support (PBS): Aims to understand the function of challenging behaviors and develop proactive strategies to prevent them.
Consistency and positive reinforcement are paramount in the success of these therapies.
Medication Management
Medication can play a role in managing ADHD symptoms.
- Stimulants and Non-stimulants: Various medications are available, each with potential benefits and side effects.
- Careful Monitoring: Regular monitoring of medication effects and adjustments as needed is crucial.
Collaboration between psychiatrists, pediatricians, and other healthcare providers ensures safe and effective medication management.
Family Support and Counseling
Strong family support is crucial.
- Respite Care: Temporary relief for caregivers to prevent burnout.
- Support Groups: Connecting with other families facing similar challenges.
- Family Therapy: Addressing emotional challenges and improving family dynamics.
The emotional toll on families is significant, emphasizing the need for professional guidance and readily available support services.
Conclusion
This comprehensive study underscores the complexities of co-occurring ADHD, Autism, and Intellectual Disability. The significant symptom overlap necessitates thorough diagnostic evaluations, while effective interventions require a multidisciplinary approach incorporating individualized education plans, behavioral therapies, medication management, and robust family support systems. Further research is needed to refine our understanding of these conditions and to develop more effective strategies. If you or someone you know is dealing with the challenges of co-occurring ADHD, Autism, and Intellectual Disability, seek professional help to develop a personalized plan for support and intervention. Understanding the nuances of co-occurring ADHD, Autism, and Intellectual Disability is crucial for creating effective interventions and improving the lives of those affected.
Featured Posts
-
 How To Purchase Capital Summertime Ball 2025 Tickets Successfully
Apr 29, 2025
How To Purchase Capital Summertime Ball 2025 Tickets Successfully
Apr 29, 2025 -
 One Plus 13 R In Depth Review And Pixel 9a Comparison
Apr 29, 2025
One Plus 13 R In Depth Review And Pixel 9a Comparison
Apr 29, 2025 -
 Search Intensifies For Missing British Paralympian In Las Vegas
Apr 29, 2025
Search Intensifies For Missing British Paralympian In Las Vegas
Apr 29, 2025 -
 I M Staying Put Schumer Rejects Speculation On Senate Leadership Succession
Apr 29, 2025
I M Staying Put Schumer Rejects Speculation On Senate Leadership Succession
Apr 29, 2025 -
 The Legacy Of Murder An Ohio Doctors Parole Hearing And A Sons Journey
Apr 29, 2025
The Legacy Of Murder An Ohio Doctors Parole Hearing And A Sons Journey
Apr 29, 2025
Latest Posts
-
 Amanda Owen On The Challenges Of Family Life On The Farm
Apr 30, 2025
Amanda Owen On The Challenges Of Family Life On The Farm
Apr 30, 2025 -
 The Challenges Of Our Yorkshire Farm Reuben Owens Perspective
Apr 30, 2025
The Challenges Of Our Yorkshire Farm Reuben Owens Perspective
Apr 30, 2025 -
 Growing Up On Our Yorkshire Farm Reuben Owens Biggest Struggle
Apr 30, 2025
Growing Up On Our Yorkshire Farm Reuben Owens Biggest Struggle
Apr 30, 2025 -
 Nine Children And A Farm Amanda Owens Family Life In Pictures
Apr 30, 2025
Nine Children And A Farm Amanda Owens Family Life In Pictures
Apr 30, 2025 -
 Our Yorkshire Farm Amanda Owen Faces Fresh Complaints Following Channel 4 Announcement
Apr 30, 2025
Our Yorkshire Farm Amanda Owen Faces Fresh Complaints Following Channel 4 Announcement
Apr 30, 2025
