Better Mental Healthcare: A Call For Systemic Reform And Increased Access

Table of Contents
Systemic Barriers to Accessing Mental Healthcare
The High Cost of Care
The financial burden of mental healthcare is a major barrier for many. Therapy sessions, medication, and hospitalization can be prohibitively expensive, leaving individuals struggling to afford the care they desperately need. This is particularly true for underserved communities who often lack adequate insurance coverage or financial resources.
- High Costs: The cost of a single therapy session can range from $100 to $300 or more, depending on the provider and location. Medication costs can also be substantial, especially for long-term treatment. Hospitalization for mental health crises can result in tens of thousands of dollars in debt.
- Impact on Underserved Communities: Low-income individuals and families, as well as those lacking adequate health insurance, are disproportionately affected by the high cost of mental healthcare. This financial barrier prevents many from seeking help, leading to worsening conditions and potentially tragic outcomes.
- Lack of Insurance Coverage: Even with insurance, many mental health services are not adequately covered, leading to high out-of-pocket expenses and limited access to specialized care. Many insurance plans have limited networks of mental health providers, further restricting access.
Shortage of Mental Health Professionals
A critical shortage of mental health professionals, including psychiatrists, therapists, and other specialists, exacerbates the access problem. This shortage is particularly acute in underserved rural and urban areas, creating significant disparities in access to care.
- Statistics on Provider Shortages: Numerous reports indicate a significant and growing gap between the demand for mental health services and the availability of providers. This leads to long wait times for appointments, limited treatment options, and decreased access to specialized care.
- Reasons for Shortages: Several factors contribute to the shortage, including burnout among existing professionals, insufficient funding for training programs, and a lack of competitive salaries. The demanding nature of the work and the emotional toll it takes on providers also contribute to this crisis.
- Geographic Disparities: Access to mental healthcare is often significantly worse in rural areas and underserved urban communities due to a lack of providers and limited transportation options.
Navigational Challenges and Stigma
Navigating the mental healthcare system can be incredibly complex and confusing for individuals already struggling with their mental health. This, combined with the persistent stigma surrounding mental illness, often prevents people from seeking help in the first place.
- Difficulty Finding Providers: Locating an appropriate and available mental health provider can be a significant hurdle. Insurance limitations, provider waitlists, and geographic constraints all contribute to the difficulty of finding care.
- Confusing Insurance Processes: Understanding insurance coverage for mental health services is often complicated, involving confusing paperwork, prior authorizations, and navigating different networks. This administrative burden can be overwhelming for those seeking help.
- Societal Stigma: The pervasive stigma surrounding mental illness discourages many individuals from seeking help, fearing judgment, discrimination, or social isolation. This stigma is a major barrier to early intervention and effective treatment.
Strategies for Systemic Reform and Increased Access
Increased Funding for Mental Health Services
Increased investment in mental health is crucial for expanding access and improving the quality of care. This funding should support a range of initiatives, from research to training programs and community-based services.
- Successful Funding Models: Examples of successful funding models include increased state and federal funding for mental health programs, targeted grants for community-based initiatives, and increased investment in research to improve treatment approaches.
- Potential Sources of Funding: Governments at all levels, as well as private foundations and corporations, should commit to increased funding for mental health services. Innovative public-private partnerships can also help leverage resources and maximize impact.
- Impact of Increased Funding: Increased funding will lead to a larger mental health workforce, expanded access to services, improved quality of care, and reduced wait times for appointments. This will ultimately improve outcomes for individuals and communities.
Expansion of Telehealth Services
Telehealth has emerged as a powerful tool for expanding access to mental healthcare, particularly in remote or underserved areas. By leveraging technology, telehealth can overcome geographical barriers and increase accessibility for many.
- Advantages of Telehealth: Telehealth offers convenience, affordability, and accessibility. Individuals can access care from the comfort of their own homes, reducing travel costs and time constraints.
- Challenges of Telehealth: Addressing the digital divide and ensuring equitable access to technology and reliable internet are crucial. Privacy concerns and the need for digital literacy among patients also need to be considered.
- Future of Telehealth: Continued investment in telehealth infrastructure and training programs for providers is vital to realizing the full potential of telehealth in improving mental healthcare access.
Addressing Mental Health in Primary Care
Integrating mental healthcare into primary care settings can significantly improve access to early intervention and treatment. This integrated approach allows for early identification of mental health issues and facilitates timely access to appropriate care.
- Models of Integrated Care: Collaborative care models, where primary care physicians work closely with mental health specialists, are effective in improving access and outcomes. Co-location of mental health providers within primary care clinics is another effective strategy.
- Training Primary Care Physicians: Training primary care physicians to screen for and manage common mental health conditions is essential. This requires increased investment in medical education and continuing professional development programs.
- Collaborative Care Models: Collaborative care models provide a structured approach to delivering mental healthcare within primary care, utilizing a team-based approach that includes primary care physicians, mental health specialists, and care managers.
Conclusion: A Call to Action for Better Mental Healthcare
The systemic barriers to accessing better mental healthcare are significant, but not insurmountable. By addressing the high cost of care, the shortage of mental health professionals, and the challenges of navigating the system, we can create a more equitable and accessible mental health system. Increased funding, expansion of telehealth services, and integrated care within primary care settings are crucial steps towards achieving this goal. Demand better mental healthcare for all. Join the movement for better mental healthcare access. Advocate for policies that prioritize mental wellness, support mental health organizations, and seek help if you or someone you know needs it. Let's work together to build a future where everyone has access to the mental healthcare they deserve.

Featured Posts
-
 The Harmful Effects Of School Suspensions Evidence And Solutions
May 02, 2025
The Harmful Effects Of School Suspensions Evidence And Solutions
May 02, 2025 -
 Kshmyr Ky Jng Fwj Ka Mstqbl Ka Mnswbh
May 02, 2025
Kshmyr Ky Jng Fwj Ka Mstqbl Ka Mnswbh
May 02, 2025 -
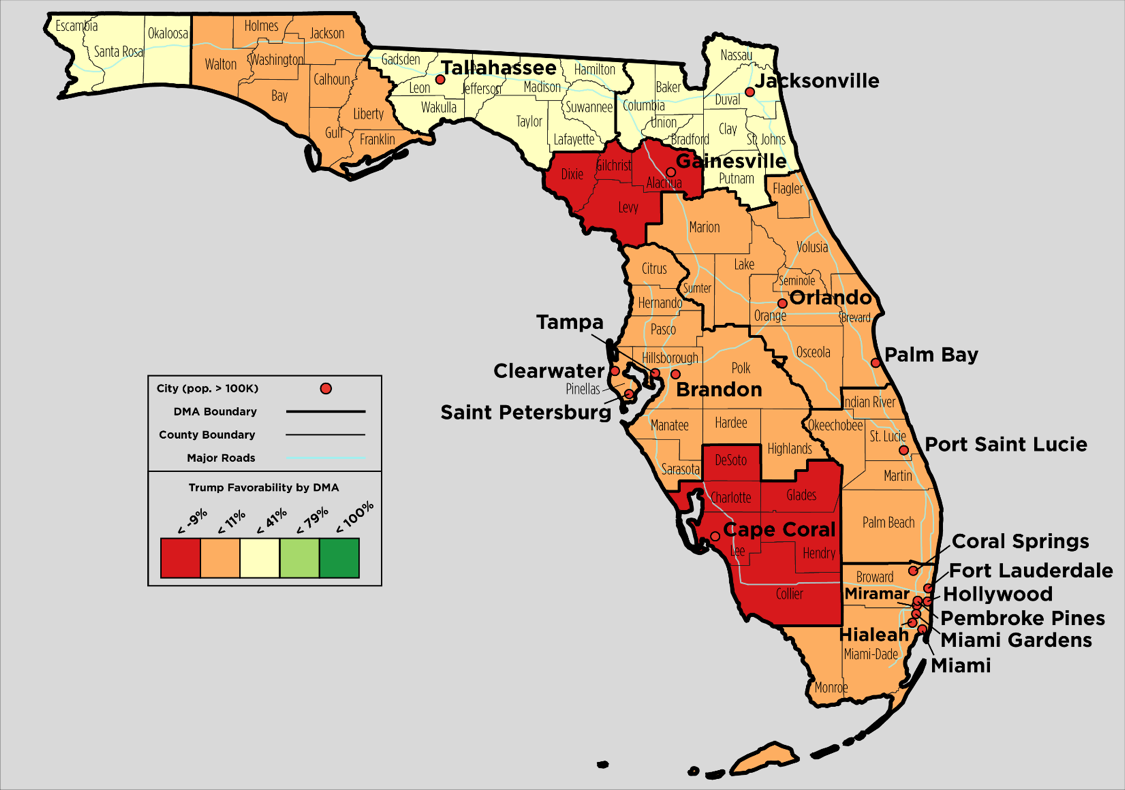 Florida And Wisconsin Turnout A Deep Dive Into The Current Political Landscape
May 02, 2025
Florida And Wisconsin Turnout A Deep Dive Into The Current Political Landscape
May 02, 2025 -
 Understanding Shrove Tuesday The Origins And Customs Of Pancake Day
May 02, 2025
Understanding Shrove Tuesday The Origins And Customs Of Pancake Day
May 02, 2025 -
 Justice Departments Decision To End School Desegregation Order Implications And Future Of Desegregation
May 02, 2025
Justice Departments Decision To End School Desegregation Order Implications And Future Of Desegregation
May 02, 2025
Latest Posts
-
 Assessing Reform Uks Credibility On Farming Issues
May 03, 2025
Assessing Reform Uks Credibility On Farming Issues
May 03, 2025 -
 Rwyt Aljbht Alwtnyt Llastthmar Thlyl Wrqt Alsyasat Alaqtsadyt
May 03, 2025
Rwyt Aljbht Alwtnyt Llastthmar Thlyl Wrqt Alsyasat Alaqtsadyt
May 03, 2025 -
 Alastthmar Fy Zl Wrqt Syasat Aljbht Alwtnyt Aljdydt
May 03, 2025
Alastthmar Fy Zl Wrqt Syasat Aljbht Alwtnyt Aljdydt
May 03, 2025 -
 Amant Alastthmar Baljbht Alwtnyt Tkshf En Khttha Alastthmaryt
May 03, 2025
Amant Alastthmar Baljbht Alwtnyt Tkshf En Khttha Alastthmaryt
May 03, 2025 -
 Astratyjyt Astthmaryt Jdydt Lljbht Alwtnyt Tfasyl Wrqt Alsyasat
May 03, 2025
Astratyjyt Astthmaryt Jdydt Lljbht Alwtnyt Tfasyl Wrqt Alsyasat
May 03, 2025
