Antibiotic Resistance: The Growing Danger Of Deadly Fungi
Table of Contents
Understanding Antifungal Resistance Mechanisms
Fungi, like bacteria, evolve resistance to antifungal drugs through various mechanisms. This adaptability poses a major challenge to effective treatment. These mechanisms include:
- Mutations: Genetic changes in fungal cells can alter the target site of antifungal drugs, rendering them ineffective. For instance, mutations in the ERG11 gene can lead to azole resistance in Candida species.
- Efflux Pumps: Fungi can develop increased expression of efflux pumps, which actively expel antifungal drugs from the fungal cell, reducing their intracellular concentration.
- Target Modification: Fungal cells may modify the target site of the drug, reducing its binding affinity and efficacy.
Here are specific examples:
- Azoles and Candida auris: Candida auris, a particularly dangerous multi-drug resistant fungus, frequently exhibits resistance to azole antifungal agents.
- Echinocandins and Aspergillus fumigatus: Aspergillus fumigatus, a common cause of invasive aspergillosis, can develop resistance to echinocandins, a class of antifungal drugs targeting the fungal cell wall.
Genetic factors and environmental influences, such as exposure to antifungal drugs in agriculture and healthcare settings, play crucial roles in driving the selection and spread of resistant strains.
The Impact of Antibiotic Resistance on Fungal Infections
A critical link exists between antibiotic use and the rise of fungal infections. Antibiotics disrupt the delicate balance of the human microbiome, suppressing beneficial bacteria that normally compete with fungi. This disruption creates an ecological niche that allows for fungal overgrowth and the subsequent development of opportunistic fungal infections.
- Increased risk of candidiasis after broad-spectrum antibiotic therapy: The use of broad-spectrum antibiotics significantly increases the risk of developing Candida infections, such as oral thrush or invasive candidiasis.
- Higher mortality rates from invasive aspergillosis in immunocompromised patients receiving antibiotics: Patients receiving antibiotics, especially those with weakened immune systems, are at a considerably higher risk of developing severe and often fatal invasive aspergillosis caused by Aspergillus fumigatus.
The increased severity and mortality associated with fungal infections in patients taking antibiotics highlight the critical interplay between antibiotic and antifungal resistance.
High-Risk Groups and Vulnerable Populations
Certain populations are at significantly higher risk of developing resistant fungal infections due to compromised immune systems or pre-existing conditions. These include:
-
Immunocompromised individuals: Cancer patients undergoing chemotherapy, organ transplant recipients, and individuals with HIV/AIDS are particularly vulnerable due to their weakened immune defenses.
-
The elderly: Older adults often have underlying health conditions and weakened immune systems, increasing their susceptibility to fungal infections.
-
Patients with pre-existing health conditions: Individuals with diabetes, chronic lung diseases, or other chronic illnesses are also at increased risk.
-
Patients undergoing chemotherapy have weakened immune systems, making them susceptible to opportunistic fungal infections. The drugs used to treat cancer often suppress the immune system, increasing vulnerability to fungal pathogens.
-
Individuals with diabetes are at higher risk of developing mucormycosis. Mucormycosis, a serious and often fatal fungal infection, is more common in individuals with poorly controlled diabetes.
Prevention and Control Strategies for Antifungal Resistance
Preventing and controlling the spread of antifungal resistance requires a multi-pronged approach:
- Responsible antifungal use: Appropriate diagnosis and targeted therapy are crucial to avoid unnecessary antifungal use and the development of resistance.
- Infection control measures in healthcare settings: Strict adherence to hygiene protocols, handwashing, and environmental disinfection can reduce the transmission of resistant fungi.
- Development of new antifungal drugs: Research and development of novel antifungal agents with new mechanisms of action are essential to combat resistance.
- Alternative therapeutic approaches: Exploring alternative therapies, such as immunotherapy or phage therapy, could offer new avenues for treatment.
Specific prevention strategies include:
- Improved hygiene practices in hospitals to reduce the spread of fungal infections.
- Development of rapid diagnostic tests for accurate identification of fungal pathogens and their resistance profiles. Early and accurate diagnosis is critical for effective treatment.
- Promoting research into novel antifungal drug targets.
The Future of Antifungal Therapy: Challenges and Opportunities
Combating antifungal resistance presents significant challenges:
- Limited number of antifungal drugs: The antifungal drug arsenal is considerably smaller than that for bacteria, limiting treatment options.
- Slow development of new antifungals: The development of new antifungal drugs is a complex and lengthy process.
- High cost of antifungal therapy: Many antifungal drugs are expensive, posing a barrier to access for some patients.
However, opportunities exist:
- Increased research and development of new antifungal drugs: Greater investment in research is crucial to develop novel antifungal agents.
- Alternative therapeutic approaches: Exploring innovative therapies, like immunotherapy or phage therapy, offers promising avenues.
- Personalized medicine: Tailoring antifungal treatment based on individual patient characteristics and fungal resistance profiles can improve treatment outcomes.
Future directions include:
- Developing new drug delivery systems: Improved drug delivery systems can enhance the efficacy of existing antifungals.
- Exploring the role of the microbiome: Manipulating the microbiome to suppress fungal growth could provide a novel therapeutic approach.
- Investing in surveillance systems: Tracking the emergence and spread of antifungal resistance is crucial for effective control.
Conclusion: Combating the Threat of Antibiotic Resistance in Fungi
The growing danger of antifungal resistance is undeniable. The interconnectedness of antibiotic and antifungal resistance underscores the urgent need for a comprehensive strategy to combat this looming threat. Responsible antifungal use, stringent infection control measures, and a renewed focus on research and development of new drugs and therapies are paramount. Understanding and addressing the growing problem of antibiotic resistance, especially concerning deadly fungi, is crucial for safeguarding public health. Learn more about antifungal resistance today and support research efforts to combat this dangerous trend. The future of effective antifungal therapy hinges on collaborative action and increased investment in research to prevent the further spread of antifungal resistance and its devastating consequences.
Featured Posts
-
 Dwp Doubles Home Visits Thousands Of Benefit Claimants Affected
May 08, 2025
Dwp Doubles Home Visits Thousands Of Benefit Claimants Affected
May 08, 2025 -
 Andor Season 2 Your Essential Guide Before The Premiere
May 08, 2025
Andor Season 2 Your Essential Guide Before The Premiere
May 08, 2025 -
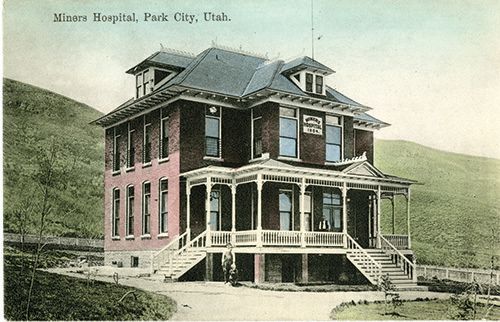 Demolition Of Historic Pierce County Home To Make Way For Park
May 08, 2025
Demolition Of Historic Pierce County Home To Make Way For Park
May 08, 2025 -
 Understanding The Papal Conclave Selection Of A New Pope
May 08, 2025
Understanding The Papal Conclave Selection Of A New Pope
May 08, 2025 -
 Tatums Candid Remarks On Larry Birds Impact On The Boston Celtics
May 08, 2025
Tatums Candid Remarks On Larry Birds Impact On The Boston Celtics
May 08, 2025
